Introduction
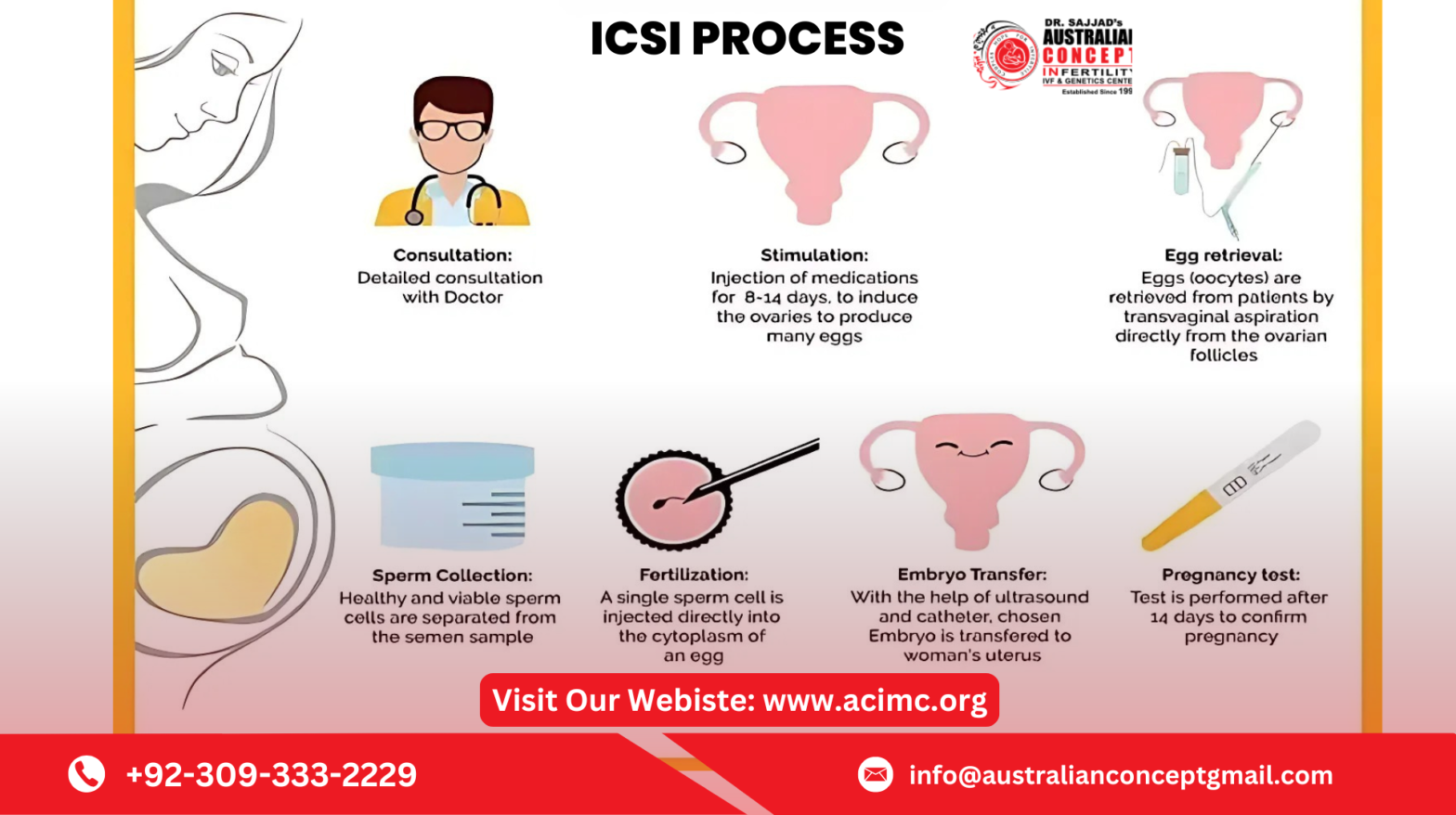
Intracytoplasmic Sperm Injection (ICSI) is a specialized form of assisted reproductive technology that has revolutionized the treatment of male infertility treatment in Pakistan. Unlike conventional IVF, where thousands of sperm are placed near an egg to promote natural fertilization, ICSI involves directly injecting a single sperm into an egg to achieve fertilization. But this technique isn’t necessary for every fertility case.
Fertility specialists assess several medical and biological factors before recommending ICSI to ensure it’s the best course of action for a successful pregnancy.
1. Severe Male Factor Infertility
ICSI is primarily recommended when a man has severe fertility issues that affect sperm quality or quantity. These include:
-
Low sperm count (oligospermia): Not enough sperm present to ensure natural fertilization.
-
Poor sperm motility (asthenospermia): Sperm can’t swim efficiently to reach the egg.
-
Abnormal sperm shape (teratospermia): Misshapen sperm are unable to penetrate the egg.
-
No sperm in ejaculate (azoospermia): When sperm must be retrieved surgically from the testicles or epididymis.
In such cases, ICSI significantly improves the chances of successful fertilization.
2. Previous Failed IVF Cycles
Couples who have gone through standard IVF cycles without successful fertilization may benefit from ICSI. Fertility specialists may recommend switching to ICSI if:
-
Fertilization fails even with good egg and sperm quality.
-
Very few or no embryos develop after IVF.
-
The couple experienced unexplained fertilization failure in the lab.
ICSI can overcome these challenges by ensuring direct fertilization of the egg with sperm.
3. Use of Frozen Sperm or Eggs
Sometimes couples use previously frozen eggs or sperm in their fertility treatments. Freezing and thawing can reduce the quality or viability of these cells. ICSI improves success rates in such cases by:
-
Helping compromised sperm fertilize the egg.
-
Ensuring fertilization even if egg membranes are slightly hardened after freezing.
This method allows couples to use preserved reproductive cells with higher confidence in positive outcomes.
4. Sperm Retrieval Procedures
When sperm cannot be obtained through natural ejaculation due to blockages, injury, or congenital conditions, surgical sperm retrieval is performed. Procedures like:
-
TESA (Testicular Sperm Aspiration)
-
PESA (Percutaneous Epididymal Sperm Aspiration)
-
Micro-TESE (Microsurgical Testicular Sperm Extraction)
These techniques yield very few and often less motile sperm. ICSI becomes essential in such cases to manually insert one viable sperm into the egg.
5. Egg-Related Issues
In some cases, female factors may also make ICSI a better option. These include:
-
Thick or hard zona pellucida (egg shell): Makes natural sperm penetration difficult.
-
Older maternal age: Aging eggs may not fertilize easily through traditional IVF.
-
Poor oocyte quality: Fertilization may require direct sperm injection.
By bypassing natural barriers, ICSI ensures fertilization even with challenging egg characteristics.
6. Unexplained Infertility
Unexplained infertility is when no clear cause is identified after standard fertility tests. Couples with this diagnosis may be advised to try ICSI if they have:
-
Spent years trying to conceive without success.
-
Experienced multiple failed IUI or IVF attempts.
-
Good egg reserve and sperm analysis but still no pregnancy.
ICSI provides a solution when all other paths have failed without explanation.
7. Preimplantation Genetic Testing (PGT)
Couples opting for PGT to screen embryos for genetic conditions may also benefit from ICSI. The reason is:
-
ICSI reduces the risk of sperm DNA contamination in embryo cells.
-
It provides cleaner, more accurate genetic analysis results.
This is particularly helpful for couples with a family history of inherited disorders.
8. Low Fertilization Rate in Previous IVF Cycles
Even if fertilization did occur in previous IVF attempts, a low number of embryos may not be enough for successful implantation. ICSI can increase the chances of producing more viable embryos for transfer or freezing.
When ICSI May Not Be Necessary
While ICSI has helped thousands of couples conceive, it’s not suitable—or needed—for everyone. Couples with:
-
Mild or no male infertility
-
Good fertilization history through IVF
-
Normal sperm parameters
may not benefit from ICSI and might achieve similar results with standard IVF. Using ICSI unnecessarily could increase costs without improving success rates.
Conclusion:
The ICSI procedure is a powerful fertility tool that offers hope to couples facing complex reproductive challenges, particularly male infertility and repeated IVF failures. However, it is not a one-size-fits-all solution. The decision to use ICSI should be based on a thorough evaluation by a qualified infertility specialist who considers all aspects of the couple’s reproductive health. With the right diagnosis and approach, ICSI can significantly improve the chances of a successful pregnancy and a healthy baby.